Tests sanguins de fibrose
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD), the liver manifestation of the metabolic syndrome linked to obesity and insulin resistance, affects 25% of the general population both in western and developing countries . NAFLD encompasses a large spectrum of liver lesions but the patient prognosis is mainly linked to the level of fibrosis which must therefore be accurately evaluated in clinical practice. In this context, non-invasive tests of liver fibrosis (blood tests, elastography) position as very interesting tools to identify the subset of patients with advanced fibrosis and impaired prognosis among the large NAFLD population. In a recent study, we have shown that liver stiffness measurement (LSM) by Vibration Controlled Transient Elastography (VCTE) and the blood test FibroMeterV were the most accurate among nine fibrosis tests evaluated to diagnose advanced fibrosis in NAFLD .
The combination of fibrosis tests significantly improves their diagnostic accuracy , but this approach remains poorly evaluated in NAFLD. Only one study has evaluated the diagnostic accuracy of an algorithm based on the agreement between VCTE and the blood test NAFLD fibrosis score (NFS) . This algorithm provided excellent accuracy for the diagnosis of advanced fibrosis in NAFLD but disagreement between both fibrosis tests occurred in half of the patient who therefore required liver biopsy. Other diagnostic algorithms combining fibrosis tests exist in chronic hepatitis C but they have never been evaluated in NAFLD. The Bordeaux algorithm is based on the agreement between VCTE and the blood test Fibrotest . The Sequential Algorithm for Fibrosis Evaluation (SAFE) combines the two blood tests APRI and Fibrotest . Such sequentia procedure is relevant for large populations in clinical practice by using a first-line test, it selects the subgroup of patients who require more complex and accurate procedures. Finally, we have developed the new and accurate FibroMeterVCTE that synchronously combines in a single formula the blood markers of the FibroMeter V with VCTE .
The aims of the present study were to evaluate in a large population of NAFLD patients the diagnostic accuracy of the fibrosis tests combinations previously developed in chronic hepatitis C; to improve the non-invasive diagnosis of advanced fibrosis in NAFLD by combining the best fibrosis tests in new practical algorithms; to evaluate the accuracy of these new algorithms in an intention-to-diagnose analysis.
PATIENTS AND METHODS
Patients
Patients with biopsy-proven NAFLD were included from January 2004 to April 2016 at Angers and Bordeaux University Hospitals. NAFLD was defined as liver steatosis on liver biopsy after exclusion of concomitant steatosis-inducing drugs, excessive alcohol consumption (>210 g/week in men or >140 g/week in women), chronic hepatitis B or C infection, and histological evidence of other concomitant chronic liver disease. Patients were not included if they had liver complications (liver failure, ascites, variceal bleeding, systemic infection or hepatocellular carcinoma).
Liver biopsy
In each center, pathological examinations were performed by a senior expert specialized in hepatology and blinded for patient data. Liver fibrosis was evaluated according to the NASH CRN scoring system , F0 no fibrosis; F1 perisinusoidal or portal/periportal fibrosis, F2 perisinusoidal and portal/periportal fibrosis, F3 bridging fibrosis and F4 cirrhosis. Significant fibrosis was defined as F≥2 and advanced fibrosis as F3/4. Because previous longitudinal studies have demonstrated that liver-related prognosis is impaired when advanced fibrosis occurs , we chose advanced F3/4 fibrosis as our primary diagnostic target.
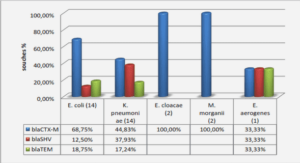
Blood fibrosis tests
Fasting blood samples were taken the day of or within the week preceding liver biopsy. The following blood fibrosis tests were calculated according to published or patented formulas NFS , FibroMeterV2G , FibroMeterV3G and FibroMeterVCTE . Wechose NFS because it is the most validated blood fibrosis test in NAFLD, and FibroMeterV2G because it was the most accurate among eight blood tests evaluated in our previous study FibroMeterV3G is the same blood fibrosis test than FibroMeterV2G but hyaluronate, a costly and difficult-to-obtain marker, has been replaced by the gammaGT . Finally, FibroMeterVCTE is a new fibrosis test that combines in a single formula the blood markers of the FibroMeterV3G with VCTE. APRI and Fibrotest were also calculated to determine the SAFE algorithm . All blood assays were performed in the laboratories of the Angers or Bordeaux centers. We have previously demonstrated the excellent inter-laboratory reproducibility of blood fibrosis tests .
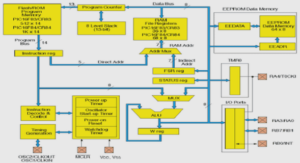
Diagnostic algorithms
The following diagnostic algorithms combining non-invasive fibrosis tests were determined (Figure s1 in Supplementary Material) SAFE, Bordeaux algorithm and Palermo algorithm As Metavir F≥2 corresponds to septal fibrosis and thus to NASH CRN F≥3 fibrosis, we used the SAFE and Bordeaux algorithms for Metavir F≥2 to diagnose advanced fibrosis in the present study. The SAFE is a sequential algorithm which includes APRI as first-line test and Fibrotest as second-line procedure. The Bordeaux and Palermo algorithms are based on the agreement between VCTE and a blood fibrosis test, respectively Fibrotest and NFS.
Statistical analysis
- Diagnostic indexes ;
Diagnostic accuracy of fibrosis tests was mainly expressed as the area under the receiver operating characteristics (AUROC) and the Obuchowski index. The Obuchowski index is a multinomial version of the AUROC adapted to ordinal references such as pathological fibrosis staging . With N (=5 F0 to F4) categories of the gold standard outcome and AUROCst, it estimates the AUROC of diagnostic tests differentiating between categories s and t. The Obuchowski index is a weighted average of the N(N-1)/2 (=10) different AUROCst corresponding to all the pair-wise comparisons between two of the N categories. In addition, the Obuchowski index was assessed using a penalty function proportional to the difference in fibrosis stages, i.e., a penalty of 1 when the difference between stages was 1, 2 when the difference was 2, 3 when the difference was 3, and 4 when the difference was 4. Finally, the result can be interpreted as the probability that the non-invasive test will correctly rank two randomly chosen patients with different fibrosis stages.
RESULTS
Patients
723 patients were included in the study, 314 in Angers and 409 in Bordeaux. 105 patients had LSM failure with the M probe. The characteristics of the 618 remaining patients included in the per-protocol analysis are detailed in Table 1. 59.1% were male, mean age was 55.2±12.5 years and mean BMI was 31.0±5.5 kg/m2 . Mean biopsy length was 27±11 mm (median 25 mm; 1st quartile 20 mm; 3rd quartile 33 mm) and 89.1% of liver biopsies had ≥15 mm length. Median LSM was 9.1 Kpa (1st quartile 6.3 kPa; 3rd quartile 14.0 kPa). Correlation and agreement between FibroMeterV2G and FibroMeterV3G were excellent with, respectively, Spearman coefficient = 0.933 (p<0.001) and intra-class correlation coefficient = 0.939 (p<0.001) (Figure s2).
Intention-to-diagnose analysis
371 patients had LSM with both M and XL probes. Their characteristics are detailed in Table s3. 67 patients had LSM failure with the M probe of whom 60 had result with the XL probe and 7 had LSM failure with both probes. Patients with LSM failure were kept in the intention-to-diagnose analysis as follow XL probe result was used in case of M probe failure, and liver biopsy was used if LSM failed with both probes. The five diagnostic algorithms (SAFE, Bordeaux, Palermo, FMV3G-VCTE and VCTE-FMVCTE) evaluated in an intention-to-diagnose basis showed similar accuracy than in the perprotocol analysis (Table 4). Figure 1 summarizes how to accurately diagnose advanced fibrosis in NAFLD in clinical practice.
DISCUSSION
As in the other causes of chronic liver diseases, an accurate evaluation of liver fibrosis is mandatory in NAFLD to decide the patient management. Liver biopsy remains the reference exam for this purpose but, because of its invasiveness, it can’t be proposed as first-line procedure to all NAFLD patients who represents 25% of the general population . Several non-invasive methods exist with their own interests and disadvantages. Blood fibrosis tests can be performed by all physicians but the most accurate include specialized and costly blood markers. VCTE is very accurate, gives an immediate result while the consultation, but remains available only in specialized centers. Other elastography methods included in Doppler-ultrasonographic devices have been developed but few data about their diagnostic accuracy and the best diagnostic cut-offs has been published. In the present work, we have developed two algorithms for the practical diagnosis of advanced fibrosis in NAFLD. We though these algorithms by considering the resources available for the physicians (either VCTE or only blood tests as first-line examination) to ensure their feasibility in clinical practice and thus their broad application. The strengths of our work are 1/ the large number of patients included, 2/ the direct comparison for the first time in NAFLD of the previously published algorithms (SAFE, Bordeaux algorithm, Palermo algorithm), and 3/ the intention-to-diagnose analysis that takes into account LSM failure and thus evaluates algorithms in the “real life” conditions. Finally, by giving the best compromise between an excellent diagnostic accuracy and the lowest rate of liver biopsy required, the new FMV3G-VCTE and VCTE-FMVCTE algorithms position as the best procedures for the noninvasive diagnosis of advanced fibrosis in NAFLD.
Conclusions
The synchronous combination of Fibroscan with blood markers in the FibroMeterVCTE improves the non-invasive diagnosis of advanced fibrosis in NAFLD. In clinical practice, the sequential use of fibrosis tests (first Fibroscan or FibroMeterV3G; then, if necessary FibroMeterV C T E) significantly reduce the need for liver biopsy.
|
Table des matières
INTRODUCTION
MÉTHODES
. Patients
. Biopsie hépatique
. Tests sanguins de fibrose
. Elastométrie impulsionnelle
. Algorithmes diagnostiques
. Analyses statistiques
RÉSULTATS
. Patients
. Comparaison des tests de fibrose
.Nouveaux algorithmes diagnostiques
. Comparaison des nouveaux algorithmes, FMV3G-VCTE et VCTE-FMV3G, avec les anciens
algorithmes publiés
. Analyse en intention de diagnostiquer
DISCUSSION ET CONCLUSION
BIBLIOGRAPHIE
LISTE DES TABLEAUX
LISTE DES FIGURES
TABLE DES MATIERES
MATERIEL SUPPLEMENTAIRE1
ABSTRACT
Methods
Results
Conclusions
![]() Télécharger le rapport complet
Télécharger le rapport complet