SAFIR-02 Lung trial
The French multicentric randomized phase II SAFIR-02 Lung trial enrolled 999 treatmentnaïve advanced NSCLC patients. Other main inclusion criteria were the absence of EGFR or ALK activating alterations, the availability of tissue sample from primary tumor or metastasis (excluding bone) suitable for molecular analysis, and the eligibility for a first-line platinumbased regimen. Patients had to undergo objective response or stability after platinum-based regimen according to RECIST 1.1. Exclusion criteria could be summarized as all the potential contraindications to one of the study drugs (Supplementary Table 1 reports the details of eligibility criteria). Regarding CNS status, only symptomatic or progressive untreated BM after the induction chemotherapy were considered as exclusion criteria. According to the study form, baseline brain MRI or CT-scan was required for every patient at inclusion. During followup, iterative brain imaging (CT-scan or MRI) was required for baseline BM-positive patients or in case of neurological symptoms.
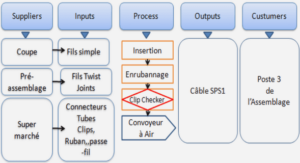
This open-label trial used high-throughput genome analysis as a therapeutic decision tool to compare experimental (arm A) versusstandard (arm B) maintenance treatments: a targeted treatment (Supplementary Table 2) versus a standard treatment if a targetable alteration was identified (substudy 1 – 175 randomized patients) or durvalumab (anti-PDL1) immunotherapy versus standard treatment in the absence of targetable molecular alteration or contraindication to targeted therapies (substudy 2 – 183 randomized patients). The standard maintenance therapy arm was based on pemetrexed for non-squamous NSCLC or erlotinib for squamous NSCLC. The substudy 1 eligibility was defined by the presence of a targetable molecular alteration according to the molecular tumor board (MTB), and molecular alterations were sorted in four categories (Supplementary Table 2). Otherwise, patients were eligible for randomization in substudy 2. The randomization was based on a 2:1 ratio in favor of the experimental arm in each substudy.
Bioinformatic analysis
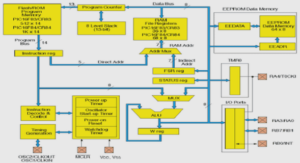
For NGS analysis, all variants passing the following thresholds were validated: depth of coverage higher than 100X, allelic ratio above 5% and population frequency lower than 0.1% in either 1000g, ESP and gnomAD. All somatic mutations were annotated, sorted and interpreted by an expert molecular biologist according to available databases (Cosmic, TumorPortal, TCGA, Cancer Hotspots…). Pathogenic variants were defined as follows: (i) for oncogenes, only mutations driving to gain of function were considered (i.e. hotspots missense mutations, in-frame insertions/deletions/splicing described as oncogenic in the literature), (ii) for tumor suppressor genes (TSG), only mutations driving to loss of function were considered (i.e. truncating alterations (nonsense mutations, frameshift insertions/deletions/splicing) or missense mutations described as deleterious in the literature).
Regarding array-CGH analysis, copy number variations from CytoScan and OncoScan were defined using the R package rCGH (v1.16.0 under R v3.6.3). Log2 relative ratios were calculated before centralization of the profile to set the baseline from which copy number alterations were estimated (two copies being the neutral level). Break points in the log2 relative ratio continuity were identified by profile segmentation. These segments were used to detect focal gene amplifications (log2 ratio >1.58, i.e. fold change >6 DNA copies; and amplicon size <10 Mb) or homozygous deletions (log2 ratio <-1) and was discussed during the tumor board. Focal amplifications and homozygous deletions were compared among the predefined groups and p-value<0.05 before adjustment was considered as statistically significant. Oncogenic driver research among regions of interest relied on two different approaches. First, the candidate strategy presumed the oncogenic driver to have been previously described as a somatic alteration in lung cancer (among a 23 genes selection) (19). Then, every potential driver was assessed with the discovery strategy, which consisted in a screen among oncoKB and Pubmed databases. Array-CGH analysis were focused on focal amplification and homozygous deletions because of their theragnostic impact compared with copy number variations analysis.
Baseline NGS analysis
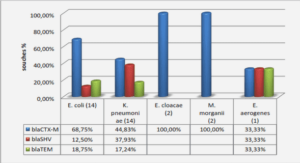
In both BM-positive and BM-negative groups, a median of two molecular variants was identified in each sample (mean 2.16 and 2.25, respectively). According to the predefined criteria (depth of coverage higher than 100X, allelic ratio above 5% and population frequency lower than 0.1% in either 1000g, ESP and gnomAD), 23 genes of the panel were selected for the analysis (ATM, BRAF, BRCA1, BRCA2, CTNNB1, EGFR, ERBB2, ERBB3, FBXW7, KEAP1, KRAS, MAP2K1, MAP2K4, MAP3K1, MET, NF1, NFE2L2, NRAS, PIK3CA, PIK3R1, STK11, TP53 and VHL). KRAS and TP53 were the most frequent altered genes in both the BM-positive (44.3% and 43.4%, respectively) and BM-negative groups (32.3% and 40.2%, respectively). Comparing the BM-positive and BM-negative populations, only KRAS mutations were found to be significantly associated with the presence of BM (p=0.005). KRAS mutation was found in 131 of the 360 patients analyzed with NGS (36.4%), including 47 patients in the BM-positive group (44.3%) and 84 in the BM-negative group (33.1%).
CNS outcome during the maintenance phase
Out of the 365 patients included in our study, 153 (41.9%) were randomized including 47 patients with baseline BM and 106 without baseline BM. Among them, 137 (89.5%) experienced disease progression before radiologic data cutoff, planned after 18 weeks of maintenance therapy. 40 out of 47 patients (85.1%) with baseline BM and 97 out of 106 patients (91.5%) without BM experienced disease progression. Brain evolution data were available for 124 out of the 137 patients who underwent disease progression. Brain progression was observed for 17 patients in the BM positive group (44.7%) and 9 patients in the BM negative group (10.5%). Occurrence of brain progression per the treatment-arm is summarized in the Figure 4a. Among the 89 randomized patients in the experimental arm (arm A of both substudy 1 and 2), 20 patients (22.5%) experienced brain progression, versus 6 out of 35 randomized patients (17.1%) in the standard chemotherapy arm (arm B of both substudy 1 and 2). Regardless of the initial BM status, the highest proportion of brain progression was identified in the durvalumab arm (Substudy 2 – Arm A), accounting for 7 CNS progression (28%) .
Focusing on KRAS mutations distribution, a G12C mutation was found for 8 patients among the 12 KRAS-mutant NSCLC patients experiencing brain progression, thus representing 66% of the mutations. On the other way, G12C mutations accounted for 38% of KRAS mutations in the non-brain progressive population (G12V 26% – G13C 24%), regardless of the initial BM status.
|
Table des matières
Article original
Résumé
Introduction
Matériel et Méthodes
Essai SAFIR-02 Lung
Population de l’étude
Analyses génomiques
Analyses bio-informatiques
Analyses statistiques
Encadrement éthique
Résultats
Population
Analyses initiales de CGH-array
Analyse des interactions protéiques
Analyses initiales de NGS
Évolution cérébrale pendant la phase de maintenance
Discussion
Bibliographie
Annexes
![]() Télécharger le rapport complet
Télécharger le rapport complet