Physiology of neural damage
Gluten sensitive neuropathies:
Gluten sensitivity is associated with multiple neurological abnormalities including gluten ataxia, peripheral neuropathy, and ischemic stroke.
Epidemiologic data:
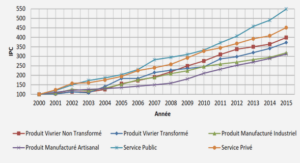
There are no accurate estimates of the prevalence of the neurological expressions of GS in the general population. Otherwise, the reported frequency of neurological abnormalities among patients with established GSE varies between 10% to 22,5% . A japanese research showed that patients with cerebellar ataxia have significantly higher rates of AGA positivity than patients without cerebellar ataxia or normal controls, which suggests that ataxic patients are more likely to have gluten sensitivity. In another study in Sheffield Hospital, UK, series of 500 patients with progressive ataxia were evaluated over a period of 13 years and showed that 46,97 % (101/215) of patients with idiopathic sporadic ataxia had serological evidence of gluten sensitivity . The prevalence of gluten ataxia was 20% among all patients with ataxias, 25% among patients with sporadic ataxias, and 45% among those with idiopathic sporadic ataxias. Otherwise, peripheral neuropathy was found in up to 23% of patients with established GSE on a gluten-free diet . Also, in a large population-based study (84.000 participants) in Sweden that examined the risk of neurological disease in patients with GSE, polyneuropathy was significantly associated with GSE (odds ratio 5,4; 95% CI 3,6–8,2) . Besides, a UK-based study showed that 47 of 140 (34%) patients with idiopathic sporadic axonal neuropathy had circulating AGA . In an Italian study, a greater proportion of patients with various types ofneuropathies were positive for IgA anti-TG2 (68 of 330 ;21%) compared with controls (1of 68; 1,5 %; p<00001). Further more, a retrospective evaluation of 400 patients with neuropathy showed the prevalence of GSE to be between 2,5% and 8% (compared with 1% in the healthy population). Finally, rare cases of ischemic stroke occurring in young adults have lead to the diagnosis of GSE .
Physiology Physiologyof neural damage of neural damage:
The search for causes of neurological dysfunction in GS has largely ignored the immunological aspect, and has concentrated on vitamin deficiencies (B12, E, D, folic acid, pyridoxine) as a result of malabsorption. Vitamin replacement rarely improves the neurological deficit. Alternative hypotheses are that antigliadin antibodies are more directly involved in the neuropathological process, or are markers of autoimmune activity with an unidentified neurotoxic antibody. If these antibodies are directly or indirectly neurotoxic, why do patients with neurological dysfunction and on gluten-free diet not always improve? One possibility is that damaged neural tissue (e.g. cerebellar Purkinje cells) does not regenerate; the second is that patients may not strictly adhere to their gluten-free diet or that the diet may be insufficient to suppress the immunological process completely, especially since patients without gastrointestinal symptoms are unlikely to adhere to a gluten-free diet . Evidence suggests there might be antibody cross-reactivity between antigenic epitopes on Purkinje cells and gluten proteins. Serum from patients with gluten ataxia and from patients with CD without neurological symptoms showed cross-reactivity with epitopes on Purkinje cells of both human and rat cerebellum.
Pathology of neural damage:
Post-mortem examination from patients with gluten ataxia showed irregular loss of Purkinje cells throughout the cerebellar cortex, which is common in many end-stage diseases of the cerebellum. However, additional findings supporting an immune-mediated pathogenesis include diffuse infiltration mainly of T-lymphocytes within the cerebellar white
matter as well as marked peri-vascular cuffing with inflammatory cells. The peripheral nervous system also showed sparse lymphocytic infiltrates with perivascular cuffing in sural nerve biopsy samples of patients with gluten neuropathy, and in dorsal root ganglia in patients with sensory neuronopathy and myopathy caused by gluten sensitivity. Similar findings have been described in patients with established celiac disease who then developed neurological dysfunction.
Serology testing:
In a genetically predisposed individual, the consumption of gluten exposes the bowel to immuno-reactive epitopes that initiate a mal-adaptive immune response . In patients with biopsy confirmed GSE, IgA antigliadin antibodies (AGA) have a sensitivity of (81%-83%)7 and a specificity of (82%-89%)7 where as the sensitivity of IgG AGA is (82-99%) and the specificity is (76%-92%). It has been proposed that AGA testing, a marker of gluten sensitivity, is an essential investigation for patients with sporadic ataxia ,and that AGA of the IgG type is the best marker for neurological manifestations of gluten sensitivity.
Patients and Methods:
Patients’ selection:
We performed a prospective study about 60 patients with different categories of idiopathic neuropathies and 57 controls. The patients were recruited at the department of neurology in the University Hospital of Marrakesh over a period of one year (from June 2010 to June 2011). Patients with known CD undergoing gluten free diet and those with etiological established diagnosis of their neuropathy were excluded from the study. The control individuals were selected from blood transfusion center affiliated to Ibn-Sina Military Hospital of Marrakesh.
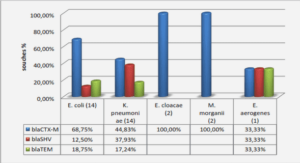
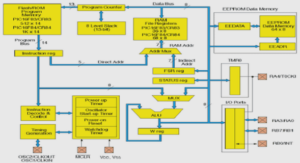
Immunologic testing:
All the patients and controls were screened for both IgG and IgA antigliadin antibodies, using an immuno-enzymological method (ELISA IgG-Gliadin, IgA-Gliadin, Diagnostic System, Germany, threshold: 12 IU/ml), followed by the anti-IgA tissue transglutaminase antibodies using the ELISA system (tGT IgA, DRG instruments, GmbH, Germany, threshold 10 IU/mL).
Statistical analysis:
All statistical analysis was performed in the laboratory of Epidemiology, Faculty of Medicine of Marrakesh, using Epi Info™ version 6.0 and SPSS program.
Ischemic stroke:
The majority of patients with GS are young, and the median of age at onset, in our series, is 40 years ranging between 25 and 74 years. Besides, case-reports about childhood stroke revealing GS have already been published. The medical record of the gluten stroke cases didn’t show any cardiovascular risk factors except 1 patient who is masculine. Also, digestive symptoms were absent for all of them. Moreover, recurrent episodes of transient ischemic strokes are reported by authors. The main clinical presentation corresponds to pure and proportional pyramidal syndrome, and rarely pseudo-bulbar syndrome, and the right side was mostly concerned in our study.
Myopathy:
AGA antibodies have been detected in various clinical forms of myopathies including proximal myopathy due to vitamin E deficiency, osteomalacia linked to vitamin D deficiency, polymyositis, juvenile form of dermatomyositis (DM) and sporadic inclusion body myositis (s-IBM). Besides, no intestinal symptoms were reported in most cases. In addition, Spanish authors found that 31% of patients with inflammatory myopathy were AGA positive and the prevalence was significantly more frequent in patients with s-IBM than DM (P<0.001). On neurologic examination, patients usually have bilateral and symmetric myogenic syndrome with progressive muscular atrophy. Moreover, the association with ataxia and neuropathy was described by some authors. Gluten myopathy can be combined to normal or increased CPK rate. On neuropathology, inflammatory myopathy is the most common finding. Finally, some authors reported an improvement of the myopathy after GFD introduction.
Epilepsy:
Epilepsy associated with GS tends to affect young patients; however, paediatric cases have also been reported. The seizures mostly resist to antiepileptic drugs, and may be benign or sometimes evolves into severe epileptic encephalopathy. The epilepsy related to GS is more often focal, besides, Magaudda and al found that the majority of patients had complex partial seizures linked to the occipital or temporal lobes. In addition, secondarily generalized seizures, or other seizure types, and episodic headaches were also described . This is in line with clinical presentation of our only positive patient who is young (44 years) and had a partial and remittent tonic-clonic status epilepticus.
Other less common manifestations:
Multiple sclerosis: An Iranian study, lead on 161 clinically defined MS patients and 166 control group who were screened for IgG and IgA antigliadin abs, showed no significant differences between MS patients and controls regarding the IgG and IgA-AGA status and anti-tTG abs as well as intestinal biopsy were negative in all positive IgG or IgA AGA. Nicoletti and al described similar observations in a case-control (217 patients vs 200 controls) Italian study . In our study, the only 1 patient with MS was positive for IgG-AGA abs and the titre was 97 IU/mL, the IgA-AGA abs and anti-tTG abs were negative.
Thrombophlebitis: A Turkish study reported 1 patient with deep venous thrombosis of the leg associated to GSE; the diagnosis was made according to the elevated rate of IgA-AGA and IgA-EMA abs along with the jejunal biopsy results. Also, Lee and Pulido described a woman with non-ischemic central retinal vein occlusion associated with GSE and suggested that hyper-viscosity due to circulating AGA abs or dehydration due to diarrhoea might cause the thrombotic event. Saibeni and al found that hyper-homocysteinemia is more frequent in patients with GSE compared with the control group, which results from vitamin deficiency caused by malabsorption and represent a risk factor for thrombosis . Similar to the Turkish study, our corresponding patient had cerebral thrombo-phlebitis and positive IgA-AGA Abs (14,32 UI/mL) but both IgG AGA and tTG were negative; unfortunately, he did not have the serum homocystein testing.
Myelopathy: Similarly to our study, among 53 unknown etiologic neuropathy patients, Hadjivassiliou included 2 cases of myelopathy. One of them had IgG-AGA abs and the other one had both IgG and IgAAGA [117]. Two patients with myelopathy were enrolled in our series and the immunological testing showed 1 positive IgG-AGA (34,25 IU/ml), but negative for both IgA-AGA and IgA-tTG.
CONCLUSION:
We conclude that serological evidence of gluten sensitivity is common in neurological diseases of unknown cause and may be etiologically linked. The diagnosis is based on AGA testing which might be the best marker for gluten neuropathies. The clinical assessment showed that peripheral neuropathy and ataxia and even ischemic stroke of young adults are commonly associated with GS. Otherwise, the effect of gluten free diet on the neuropathy will be an additional argument for this association and, therefore, offers the prospect of a realistic therapeutic possibility for some untreatable neuropathies. Indeed, further studies with larger sampling of patients as well as experiments on the effectiveness of the gluten free diet are strongly needed.
|
Table des matières
Introduction
Definitions
Gluten sensitive enteropathy
Historical review
Physiopatholog3
Epidemiology
Diagnosis
Gluten sensitive neuropathies
Epidemiological data
Physiology of neural damage
Pathology of neural damage
Neurological categories
Serology testing
Patients and Methods
Results
Global data
Ischemic stroke
Peripheral neuropathy
Ataxia
Epilepsy
Myopathy
Myelopathy
Cerebral thrombophlebitis
Multiple sclerosis
Other neurological conditions
Discussion
Relevance of immunological testing
Socio demographic characteristics of the positive cases
Epidemiological analysis
Clinical and investigations data
Immunological Investigations
Conclusion
![]() Télécharger le rapport complet
Télécharger le rapport complet