Characteristics of the whole cohort
Intermediate evaluation
Endocrine disorders
Sixty seven patients had one or more endocrine disorders between the end of BB-SFOP chemotherapy and last evaluation: twenty seven developed central precocious puberty, thirty one GHD, thirty seven thyrotropin deficiency, nineteen corticotrophin deficiency, eight hypogonadotropic hypogonadism, and seventeen central diabetes insipidus.
Subsequent therapies
Seventy-four patients completed BB-SFOP chemotherapy regimen, 13 stopped before the end because of tumor progression, 8 because of no tumor response (all received subsequent surgery and/or radiotherapy and/or chemotherapy treatment), 1 because of chemotherapy toxicity, 2 for parental refusal and 4 for other reasons. Mean duration of BB-SFOP chemotherapy was 12.7 ± 5.6 months.
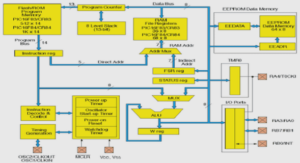
Thirty-one patients received only BBSFOP-chemotherapy. In 59 patients, one to eight courses of subsequent chemotherapy was administered following BB-SFOP chemotherapy. Chemotherapy courses applied after BB-SFOP chemotherapy included Packer regimen (Vincristine and Carboplatin), Vinblastine, SIOPP LGG, BevacizumabIrinotecan, Hydroxyurea, Cisplatin-Etoposide, Temozolomide, TPCV (Thioguanine, Procarbazine, Lomustine, and Vincristine), Vinolo protocol (Vinblastine and Nilotinib),among others. Thirty five patients needed radiotherapy after BB-SFOP chemotherapy because of tumor progression, at a mean age of 9.03 ± 4.01 years, with radiation doses ranging from 44 to 56 gray. Thirty-one patients required surgery after BB-SFOP chemotherapy (for partial or subtotal tumor resection). The details of all subsequent therapies applied after BB-SFOP chemotherapy was shown in Figure 3 (and in a supplementary Table in Annexe II).
In addition, thirty six patients required a shunt and/or shunt revision (from one to nine procedures) for intracranial hypertension performed before, during or after BB-SFOP chemotherapy. Their association with late obesity and late endocrine disorder(s) were shown Figure 4.
Late evaluation
Clinical characteristics of the patients at last evaluation The mean time between the diagnosis and last evaluation was 13.9 ± 3.7 years. Mean age at final evaluation was 17.1 ± 4 years. Four patients died after the endocrine evaluation, between the age of 14.7 and 22.7 years old, because of tumor progression (all had endocrine disorder(s): one with GHD, one with corticotrophin deficiency, one with central diabete insipidus and one with combined central diabete insipidus and thyrotropin and corticotrophin and gonadotropin deficiencies). Clinical characteristics and endocrine disorders at last evaluation were detailed in Table II. Twenty-five males and twenty-six females were at adult height at last clinical evaluation: mean adult height and weight were 1.68 ± 0.08 m (-1.1 ± 1.3 SDS) and 79.4 ± 31 kg (1.1 ± 4.5SDS) in males and 1.58 ± 0.08 m (-0.7 ± 1.4 SDS) and 64.4 ± 19.1 kg (2.1 ± 3.4SDS) in females: 15.4% of females and 20% of males had adult height two or more standard deviations below population norms.
A history of central precocious puberty was found in 36% of children. GHD was the most frequent deficiency, with 74% of patients affected, and followed by 57% of thyrotropin deficiency, 36% of corticotrophin deficiency, 33% of hypogonadotropic hypogonadism, 30% of hypergonadotropic hypogonadism, and 15% of central diabetes insipidus. Male and female appeared to be equally affected by endocrine disorder except for hypergonadotropic hypogonadism where male gender is more represented. Endocrine disorders are detailed in Figure 5.
Biological characteristics of the patients at last evaluation
Biological characteristics of patients at last evaluation were detailed table IV.
GHD was significantly associated with radiotherapy in univariate analysis and less associated with age between 2,5 and 4 years at diagnosis and chemotherapy alone in univariate and multivariate analysis.
Thyroptropin deficiency was significantly associated with intracranial hypertension at diagnosis, radiotherapy, surgery and radiotherapy and surgery, and less associated with BB-SFOP chemotherapy only, chemotherapy alone and NF1 in univariate analysis. In multivariate analysis, thyroptropin deficiency was significantly less associated with NF1 and chemotherapy alone.
Corticotrophin deficiency was significantly associated with cachexia, radiotherapy, surgery, and procedures for intracranial hypertension in univariate analysis. In multivariate analysis, corticotrophin deficiency was significantly associated with intracranial hypertension and age younger than one year old at diagnosis and less associated with chemotherapy alone.
Hypogonadotropic hypogonadism was significantly associated with radiotherapy and surgery in univariate analysis and less associated with chemotherapy alone, in multivariate analysis.
Hypergonadotropic hypogonadism was significantly associated with male, NF1 and chemotherapy alone in multivariate analysis, and less associated with radiotherapy and surgery in univariate analysis.
Central diabetes insipidus was significantly associated with cachexia, radiotherapy and surgery and radiotherapy, in univariate analysis, and with surgery in multivariate analysis. Central precocious puberty was significantly associated with younger age at diagnosis (under the median age which was 2.58 years) in multivariate analysis.
Obesity was significantly associated with intracranial hypertension at diagnosis and surgery and radiotherapy, in multivariate analysis and was less associated with chemotherapy alone in univariate analysis.
DISCUSSION
Our main findings were a high rate of endocrine disorder with 94.1% of children with OPG treated with upfront chemotherapy who developed at least one deficiency during follow-up. There was a long period of follow-up in our study (mean time: 13.9 ± 3.7 years). GHD was the most frequent deficiency, with 74% of patients affected, followed by 57% of thyrotropin deficiency, 36% of corticotrophin deficiency, 36% of history of central precocious puberty, 33% of hypogonadotropic hypogonadism, 30% of hypergonadotropic hypogonadism, and 15% of central diabetes insipidus. Multiple pituitary deficiency was the rule with 92% of the patients with two or more deficiencies.
Anatomical location on initial MRI was not predictive of late involvement.
Chemotherapy only (either BB-SFOP only or BB-SFOP + subsequent chemotherapy) was protective of late endocrine involvement.
This high incidence of hypopituitarism underscores the need for life-long endocrine follow-up and appropriate replacement.
At last evaluation 46% of patients had obesity (BMI > 2 SDS). We found here that the frequency of obesity increased with time (shown in Annexe III). Late metabolic effects as obesity and its consequences have been well described after childhood cancer therapy. The frequency of obesity varies between 35% to 53%; however studies included several low grade gliomas (LGG), not specifically OPG, and the main treatment were radiotherapy and surgery [15, 22, 31, 51]. It has been showed that tumor location in midbrain/optic nerve was related to earlier weight gain compared with other tumor sites [21]. Intracranial hypertension at diagnosis and subsequent radiotherapy and surgery appeared to be predictors of obesity in our study. To our knowledge, intracranial hypertension at diagnosis has never been described as a predictive factor of long term obesity. Moreover, GH, thyrotropin and corticotrophin deficiencies favor weight gain. Early nutritional care is likely to be of crucial importance to limit later obesity. Our patients with OPG treated by upfront chemotherapy had reduced adult height at -1.1 SDS in men and -0.7 SDS in women. In our study, 15.4% of women and 20% of men had adult heights two or more standard deviations below population norms which was quite higher than brain tumor survivors enrolled in Childhood Cancer Survivor Study cohort (with 13% of adult having short stature) [24]. Our patients had -1.75±2.1 SDS mean delta height between diagnosis and last evaluation, this was not described in the hypothalamic/chiasmatic LGG study comparing 2 groups with and without radiotherapy (with respectives mean delta height of -0.36±0.3 and -0.11±0.3 SDS) but the median time of follow-up was 3.6 years, and long term data were lacking [31]. A high rate of GHD (74%) was found in our study, versus 29% to 40% in the literature of childhood brain tumor [20, 22, 31, 52]. These discrepancies may be due to the heterogeneity of type of cranial tumors as well as of treatments reported in the literature. In addition, follow-up was generally shorter in published studies. Chemotherapy has been associated with earlier decrease in IGF1 level (after the mean 20.2 months), and GHD occurred among earliest pituitary deficiencies [21]. Radiotherapy was associated with GHD in our study, which has been well established in literature, and been explained by the fact that GHrH neurons are the most radiosensitive of the axis. However younger age at diagnosis has already been associated with later short stature. This was not the case in our study (GHD was less associated with age between 2.5 and 4 years), likely because the mean age at diagnosis was already young (3.26±0.3 years) and the frequency of GHD was high.
In literature, the occurrence of central precocious puberty was reported in 26% of children with OPG followed up for 8.3 (0.04-26.8) years [22]. In our study, the frequency was higher with 36% of children; this could be explained by the fact that our population was younger at diagnosis and follow-up longer. Thirty eight percent of our central precocious puberty cases occurred among patients with NF1 which is comparable to literature with 39% of children with chiasmal OPG develop precocious puberty [53].
These findings underscored the need to have regular assessments of growth and puberty in those children. Early treatment of precocious puberty may provide additional benefit to adult height. The occurrence of central precocious puberty was not associated with later endocrine involvement in our study and we have not highlighted an association between central precocious puberty and hypergonadotropic hypogonadism as described by others [51].
We found that NF1 status was a protective factor in univariate analysis, whereas intracranial hypertension at diagnosis and cachexia were associated with a higher risk of developing thyrotropin and corticotrophin deficiencies. NF1 has been associated with less aggressive OPG and better overall survival, while intracranial hypertension and cachexia have been associated with a worse prognosis [5, 14, 18]. Up to now, NF1 has not been well established as a protective factor for endocrine involvement [31]. In literature OPG associated with NF1 are considered to have a more indolent course, the radiologic progression, visual deterioration, and endocrine complications were documented more commonly in children with sporadic tumors than in those associated with NF1 [54].
However, the presence of diencephalic syndrome (defined as cachexia) was described to be more predictive of endocrine dysfunction (central precocious puberty and pituitary deficiencies) than treatment related factors such as radiotherapy [31]. In our study, cachexia was significantly associated with central diabetes insipidus, and corticotrophin deficiency in univariate analysis. Otherwise procedures for intracranial hypertension (shunt and/or shunt revision) were significantly associated with hypergonadotropic hypogonadism and corticotrophin deficiency in univariate analysis but not in multivariate analysis. This finding likely suggests watching carefully the children with initial intracranial hypertension, whether requires shunt or not, and cachexia, as they displayed a high risk of long term complication.
Younger age at diagnosis has already been described as a worse prognosis factor in term of overall survival and tumor progression [5, 16]. In our study, we found significant association between younger age and central precocious puberty and corticotrophin deficiency. In a recent study analyzing centrally located low grade glioma (comprising optic pathway glioma) with mostly chemotherapy as initial treatment, a significant association between age and growth hormone deficiency and hypothyroidism has been revealed [40]. This was not the case in our study likely because those deficiencies (GHD and hypothyroidism) had high frequency. This study also showed a strikingly high incidence of neurocognitive abnormalities and endocrinopathies associated with younger age and conclude that efforts to avoid or delay radiotherapy in younger patients still resulted in long term endocrine disorder [40]. This was the case in our study, subsequent radiotherapy was used as salvage therapy, and avoided in young children (mean age at administration was 9.03 ± 4.01 years) and was still associated with high incidence of late endocrine disorder (GHD, thyrotropin, corticotrophin and gonadotropin deficiencies, and central diabetes insipidus). This confirms the suggestion that even when radiotherapy is delayed with the initial use of chemotherapy in young children, they are still vulnerable to the long-term effects of irradiation [40].
The rates of thyrotropin (57%) and corticotrophin (36%) deficiencies in our study appeared higher than those described in the literature, with respectively 13-33% and 12- 26% deficiencies at 15 years of age in the study by Armstrong about low grade cranial glioma (including 7.5% optic glioma among 361 patients)[20][22, 31]. We believe that these discrepancies could be explained by the exclusive report of symptomatic OPG in our study.
When more than one axis was involved, ccorticotrophin deficiency and central diabetes insipidus appeared to be the latest axis affected. We could hypothesize this is due to the localisation of CRH (Cortisol Releasing Hormone) neurones in the paraventricular nucleus which are located the furthest from the chiasma. Moreover, part of AVP secretion (involve in central diabetes insipidus) can occur from paraventricular nucleus.
Percentages of long term hypogonadotropic and hypergonadotropic hypogonadism were respectively 33.3% and 29.8% in our study. Hypogonadotropic hypogonadism has been described in 20-36% of children with low grade glioma in the literature [22, 31].
Hypergonadotropic hypogonadism was less frequently reported in literature. Radiotherapy and surgery applied after BBSFOP chemotherapy was associated with an increased risk of hypogonadotropic hypogonadism, whereas chemotherapy only (either BB-SFOP only or BB-SFOP + subsequent chemotherapy) was associated with an increased risk of hypergonadotropic hypogonadism. This likely reflected a direct effect of radiotherapy and surgery as well as more progressive OPG with direct tumoral effect on the hypothalamic-pituitary area. Surprisingly, subsequent radiotherapy and surgery were apparently protective against hypergonadotropic hypogonadism in our study. This may be due to a protective effect on gonadal function of a silenced gonadotropin function, therefore limiting direct gonadal toxicity of chemotherapy. Alternatively, cranial radiotherapy could only hamper the increase of circulating FSH and LH levels owing to direct gonadal toxicity of chemotherapy, therefore masking the diagnosis of hypergonadotropic hypogonadism. Further studies will be necessary to assess fertility in these subjects. In addition, fertility preservation might be important to discuss as early as possible in these subjects. Males were more exposed to hypergonadodotopic hypogonadism than females in our study, therefore suggesting that BB-SFOP chemotherapy was more toxic for the testis than the ovary. Carboplatin, cisplatin and cyclophosphamide (included in the BB-SFOP protocol) have been described to cause gonadal failure [26, 27], and chemotherapy-related gonadal toxicity was generally more frequent in males as compared to females [28].
Gan, among others, described hypothalamic involvement as a predictor of earlier endocrinopathies more than treatment [31], this was not the case in our study likely because a high rate (90.4%) of patients had hypothalamic involvement on diagnosis MRI.
We did not identify any MRI location in multivariate analysis as predictive factor likely because almost all of our population (97.6%) had chiasmatic and/or hypothalamic involvement. Further studies are necessary to assess location as predictive factors on late endocrine disorders.
Management of symptomatic OPG remains controversial [4, 56, 57]. Numerous studies were concern with overall survival and ophthalmological outcome [5, 58, 59]. Late endocrine sequelae and its consequences, resulting from tumor involvement and/or therapy used (chemotherapy, surgical and/or irradiation treatment), were less described or using small cohort, heterogeneous group of tumor, or follow-up probably not long enough. We described a high rate of late endocrine disorders in this patient, higher than other brain tumor location, and because consequences are not negligible in term of quality of life (obesity, short stature, long life therapies, and psychological repercussions) this endocrine outcomes need to be closely and life-long monitored in this patients, and appropriate replacement treatment should be initiated as earlier as possible. Our main finding was the protective role of chemotherapy only (BB-SFOP only or BB-SFOP + subsequent chemotherapy) on late endocrine involvement, either because reflecting less progressive OPG, or because radiotherapy and/or surgery were not required.
There was limitation in this study that should be acknowledged. The study included only children treated for progressive OPG, and excluded children with asymptomatic OPG that did not justified treatment: we focused on the more severe OPG, hence the high rate of late endocrine dysfunction. A second limitation of this study is the lack of histological diagnosis. Most studies concerning optic pathway glioma have reported a histological diagnosis in a limited number of patients, and the diagnosis was usually established based on MRI, especially for patients with NF1.
In conclusion, obesity and late endocrine dysfunction were frequently found in subjects treated by upfront chemotherapy for OPG during childhood. Chemotherapy when used alone was protective of endocrine sequelae, further underlining that the avoidance of radiotherapy and surgery, if possible, may spare pituitary function.
|
Table des matières
LISTE DES ABREVIATIONS
ABSTRACT
INTRODUCTION
PATIENTS AND METHOD
RESULTS
1. Description of the cohort
1.1. Characteristics of the whole cohort
1.2. Characteristics of the patients at diagnosis and at the end of BB-SFOP chemotherapy
1.3. Cranial MRI characteristics of the 102 patients at diagnosis
2. Intermediate evaluation
2.1. Endocrine disorders
2.2. Subsequent therapies
3. Late evaluation
3.1. Clinical characteristics of the patients at last evaluation
3.2. Biological characteristics of the patients at last evaluation
4. Early predictors of endocrine involvement
DISCUSSION AND CONCLUSION
REFERENCES
LISTE DES FIGURES
LISTE DES TABLEAUX
TABLE DES MATIERES
ANNEXES
![]() Télécharger le rapport complet
Télécharger le rapport complet