Cadre théorique
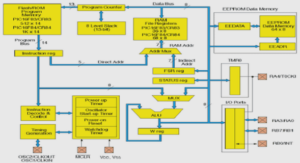
Cette étude s’inspire de la proposition théorique des tâches et compétences essentielles d’autogestion de Lorig et Holman (2003). Ce modèle provient de la discipline infirmière, ce qui le rend d’autant plus pertinent pour ce mémoire. Le concept d’autogestion a été décrit comme comportant trois domaines de tâches d’autogestion, soit la gestion médicale (la prise de médicament, le suivi d’un régime spécial, l’utilisation d’un inhalateur, ect.), la gestion émotionnelle (qui consiste à faire face aux séquelles émotionnelles de l’état chronique) et la gestion de rôle (où la personne doit s’impliquer afin de maintenir, de modifier et de créer de nouveaux comportements) (Lorig & Holman, 2003). Ces mêmes auteurs ont également soulevé, à partir d’une revue de la littérature, que l’autogestion requiert six compétences essentielles, soit la mise en action (apprendre à poser des actions dans le but de changer un comportement, un état), la prise de décisions (prendre des décisions au quotidien en réponse à l’évolution de leur maladie), le développement d’un partenariat patient-intervenant (être en mesure de former un partenariat avec leurs professionnels de la santé), l’auto-adaptation (utiliser les compétences d’autogestion et savoir les appliquer à soi-même comme il convient), l’utilisation des ressources (capacité à trouver les bonnes ressources pour les accompagner dans le suivi de leur condition chronique) et la résolution de problème (réussir à définir le problème, à générer des solutions possibles avec l’aide de la famille et des professionnels de la santé, les mettre en oeuvre et évaluer les résultats) (Lorig & Holman, 2003). La Figure 1 représente le modèle théorique de l’autogestion de Lorig et Holman (2003).
Cette proposition théorique a servi de cadre de référence permettant d’appréhender les différents aspects de l’autogestion à examiner chez la clientèle ayant des besoins de santé complexes tant au plan de l’analyse thématique de la littérature à la base de la recension des écrits de ce mémoire qu’au plan de la collecte et de l’analyse des données empirique auprès de cette population.
Pour bien gérer sa maladie, la personne a initialement besoin du soutien des professionnels de la santé (Lorig & Holman, 2003). Ainsi, cette recherche est fort pertinente pour la discipline infirmière puisque selon la définition de Pepin, Ducharme et Kerouac (2017) : « La discipline infirmière s’intéresse au soin, dans ses diverses expressions, auprès des personnes, des familles, des communautés et des populations qui, en interaction continue avec leur environnement, vivent des expériences de santé. » (p. 16). En ce sens, pour être en mesure de bien accomplir son rôle soit; de bien soutenir la personne dans ses besoins d’autogestion, l’infirmière doit bien connaître les caractéristiques de ce concept chez les personnes ayant des besoins de santé complexes. Les infirmières sont des actrices clés dans le soutien à l’autogestion et se doivent d’être éclairées sur ce concept auprès de cette clientèle spécifique (Association des infirmières et infirmiers autorisés de l’Ontario, 2015).
But de l’étude et question de recherche
Cette étude a pour but de décrire les particularités de l’autogestion des personnes ayant des besoins de santé complexes afin d’améliorer les connaissances en sciences infirmières en lien avec le soutien à l’autogestion de cette clientèle. La question de recherche est la suivante : Quelles sont les particularités de l’autogestion des personnes ayant des besoins de santé complexes ?
Abstract
Objective The management of a complex health issue may lead to important self-management challenges. There is a gap of knowledge among healthcare providers on the ways to offer self-management support to patients with complex needs. Consequently, the objective of this paper was to identify characteristics of self-management among patients with chronic diseases and complex healthcare needs.
Design Thematic analysis review of the literature
Methods We developed search strategies for the Medline and CINAHL databases, covering the January 2000-October 2018 period. All articles in English or French addressing self-management among an adult clientele (18 years and older) with complex
healthcare needs (multimorbidity, vulnerability, complexity, frequent use of health services), were included. Studies that addressed self-management of a single disease, or that did not have any notion of complexity or vulnerability were excluded. A thematic analysis was performed on the results of all articles by three evaluators as described by Miles, Huberman & Saldana (2014).
Results Twenty-one articles were included. Patients with complex healthcare needs present specific features related to self-management that can be exacerbated by deprived socioeconomic conditions. These patients must often prioritize care based on one dominant condition. They are more at risk for depression, psychological distress and low self-efficacy, as well as for receiving contradictory information from healthcare providers. On the other hand, the knowledge and experiences acquired in the past in relation to their condition may help them improve their self-management skills.
Conclusions This review identifies challenges to self-management for patients with complex healthcare needs, which are exacerbated in contexts of socio-economic insecurity, and proposes strategies to help healthcare providers better adapt their self-management support interventions to meet the specific needs of this vulnerable clientele.
Strengths and limitations of this study
– The analysis was conducted using a recognized conceptual model of self-management.
– There is a lack of consensus in the literature regarding the definition of patients with complex needs, so we ensured that the selection criteria developed for this study were broad enough to include a range of definitions for complexity.
– A limitation of any review is the potential omission of relevant articles as well as any unpublished material.
Introduction
A great majority of patients who consult the healthcare system worldwide present one or more chronic diseases (Bayliss, Bosworth, et al., 2007). Responsible for 63% of deaths, chronic diseases represent the first cause of mortality in the world (Organisation Mondiale de la Santé, 2017). Characterized by periods of stability and deteriorations, the health condition of people with chronic diseases requires constant attention by the persons who are affected, as well as by those who surround them, in order to manage symptoms and consequences. Persons living with chronic diseases must develop self-management skills.
Self-management has been defined as “the practice of activities that individuals initiate and perform on their own behalf in maintaining life, health, and well-being” and “developing the skills needed to devise, implement, evaluate, and revise an individualized plan for lifestyle change” (Orem, 1991). Self-management incorporates an array of skills that a person must possess in order to take charge of his or her health. Lorig and Holman (Lorig & Holman, 2003) developed a theoretical model for self- management involving three self-management tasks: medical management, emotional management and role management. According to this model, self-management requires six self-management skills in the patient: decision-making, action-planning, development of a patient–provider partnership, self-tailoring, resource utilization, and problem solving.
To date, self-management has mainly been studied in the context of a specific chronic disease, even though the management of a more complex health issue may lead to important self-management challenges (Bardach et al., 2011; Bayliss, Ellis, et al., 2007). Therefore, there is a gap in knowledge on the ways to offer self-management support to patients with complex needs (Sevick et al., 2007). Providers constantly work with this clientele whether it be in hospitals, emergency services, medical clinics, in homecare, etc. Thus, they play an important role in self-management support (Association des infirmières et des infirmiers autorisés de l’Ontario, 2010) . However, the scarcity of knowledge on the specifics of self-management among these complex patients can be detrimental to healthcare providers’ capacity to adequately support and accompany such patients in the self-management of their chronic conditions. Consequently, it is important to increase our understanding of the characteristics of self-management for this clientele, for whom the current norm for care in regards to the management of a single disease may not be appropriate (Bayliss, Bosworth, et al., 2007).
The aim of this paper was to review the literature to identify the characteristics of self- management among patients with chronic diseases and complex healthcare needs.
Methods
Design
A review of the literature including quantitative, qualitative and mixed studies was conducted on papers addressing the self-management of persons with complex healthcare needs. We followed the same synthesis process of the thematic analysis published in 2012 by Hudon et al.
Search methods
We conducted an electronic literature search in the Medline and CINAHL databases, for articles in English and in French published between January 2000 and October 2018. An information specialist developed and ran the specific search strategies for each database. The following MeSH terms and keywords were used: self-care OR self-management OR self-monitoring AND multimorbidity OR comorbidity OR vulnerability OR complex* OR multiple chronic diseases OR multiple chronic conditions OR frequent users OR high users. We also examined articles found in the reference lists of collected articles (hand search).
Data collection
All search results were transferred to the Endnote X7 reference software and duplicates were eliminated. Articles retained had to respect the following criteria: (1) refer to self- management, (2) among a clientele with complex healthcare needs (multimorbidity, vulnerability, complexity, frequent use of health services), and (3) in a population of patients eighteen years and older. One team member (APGL) read all titles and abstracts to exclude articles that were clearly not eligible. We excluded references that did not meet our inclusion criteria and retained all other references for complete evaluation. Two reviewers (APGL and CH or APGL and MCC) independently appraised the full text of the retained papers to identify potentially eligible articles. Discrepancies between the two reviewers regarding the inclusion or exclusion of papers were resolved by the third evaluator.
Analysis and synthesis
A three-stage review and thematic analysis of qualitative, quantitative and mixed-methods similar to Hudon et al. (2012) was undertaken (Hudon et al., 2012). First, the literature was reviewed and all selected articles were imported into the NVivo 11 qualitative analysis software. Second, analysis was performed on the results of the articles by three evaluators as described by Miles, Huberman et Saldana (2014) (Miles, Huberman, & Saldana, 2014) with the Lorig and Holman model (three self-management tasks and six self-management skills) as a guide (Lorig & Holman, 2003). Excerpts were extracted from each of the reviewed articles and classified according to the self-management skills and tasks particular to patients with complex care needs. Third, a second reading of the collected excerpts and familiarization with the data allowed for the identification of emergent themes. Pair debriefing, and team validation minimized the influence of researcher subjectivity and preconceptions (Creswell, 2006). This was an iterative process where interpretations of the data extracted from the articles were validated, and where disagreements or questions were discussed and resolved by consensus among the three evaluators.
Results
Included studies
Figure 1 shows the number of references found at each stage of the selection process. The search strategies identified 1192 references, of which 980 were kept after removing duplicates. The majority of these references were rejected because they addressed the self-management of a single disease and did not contain any notion of complexity. References found through hand searching (n = 3) were also included, for a total of 60 potentially eligible references. Sixty papers were read completely. Of these, 38 articles were excluded after the full reading step: 15 did not contain any notion of complexity in the studied population; 11 did not address self-management; 9 did not address the challenges of self-management; 1 was an editorial and 2 articles were on the validation of a measuring tool. A final sample of 22 articles was retained. Table 1 presents the characteristics of the included articles.
Characteristics of self-management by patients with complex health needs
Five main themes emerged that describe the distinctive features of self-management in these patients.
Need for prioritization of self-care. Prioritization of self-care is an important self-management challenge for patients with multiple chronic diseases. When the number of self-care activities or tasks to accomplish surpasses the amount of time available, patients will establish a daily plan around the management of their chronic conditions (Restorick et al., 2017), and must inevitably determine which self-care activities to prioritize. Patients with multimorbidity prioritize self-care activities based on the identification of one dominant condition (Bratzke et al., 2015).
Three types of conditions are more frequently identified as a dominant condition: a poorly controlled condition that tends to cause important exacerbations or negatively affect the control of other conditions, a condition that cannot be controlled solely by medication, or an unstable condition for which it is impossible to anticipate daily self-management needs. The patient is more likely to adopt a self-management strategy if he or she thinks that it will benefit more than one condition (Bayliss, Ellis, et al., 2007; Bower et al., 2013; Leach & Schoenberg, 2008).
Lack of motivation and greater risk for depression. Patients with complex needs may experience less energy, and lack time and motivation to take part in self-management activities (Coventry et al., 2014; Hill et al., 2013). They report feelings of sadness, anger and anxiety related to their illness (Restorick et al., 2017). They are more at risk for depression (Hill et al., 2013). The emotional impact of disease can play an important role in decision-making. A depressive state may give patients the impression that they will never be capable of participating in self-management activities (Bratzke et al., 2015; Morris et al., 2011). Even when patients are committed to adopting healthier lifestyle habits, they admit that depression could delay them from taking action (Coventry et al., 2014; Harrison et al., 2012; Hill et al., 2013). If they focus on their inability to control a situation, patients tend to ruminate on the negative aspects of their health status and sink into emotional distress which prevents them from taking appropriate action when faced with a problem (Leach & Schoenberg, 2008).
Increased risk of presenting poor self-efficacy. Self-efficacy is an important mediator of taking action. People’s beliefs about their own self-efficacy reflect “their capabilities to produce designated levels of performance that exercise influence over events that affect their lives” and determine how they “feel, think and motivate themselves and behave” (Bandura, 1994). Patients presenting numerous comorbidities are more at risk of presenting poor self-efficacy (Harrison et al., 2012). A person with low self-efficacy may experience difficulty in taking action to change lifestyle habits or in preventing the exacerbation of symptoms, leading to frequent hospital visits (Gallagher et al., 2008).
Patients living in situations of poverty often perceive that their poor health status is the norm, which greatly limits their motivation to improve their health (Coventry et al., 2014). Patients with multimorbidity living in underprivileged neighborhoods have lower expectations in regard to health and aging than patients from privileged neighborhoods (Coventry et al., 2014). Increased risk of receiving conflicting information. Patients with complex care needs are more at risk of receiving conflicting information on the management of their diseases by the numerous health professionals that they meet (Bayliss, Bosworth, et al., 2007; Liddy et al., 2014; Morris et al., 2011). This can lead to increased anxiety and decreased self-management capacity (Bower et al., 2013).
A personalized evaluation of learning capacity, behavior change and the desire to commit to self-management, as well as regular monitoring, facilitates patient self-management. Initiating too many changes at one time may overload the patient and his or her self-management capacity (Bayliss, Bosworth, et al., 2007; Liddy et al., 2014). Treatment goals should be selected based on patient motivation and willingness to change (Noel et al., 2007).
Opportunity to use personal experience. Complex healthcare needs do not necessarily require a new set of practices for each new diagnosis. Patients with complex care needs can use the knowledge and personal experience acquired in the past and apply them in various situations to better manage their health (Liddy et al., 2014; Morris et al., 2011). However, economic hardship reduces structural and emotional capacity, which may often prevent people living in economically precarious areas from adopting self-management behaviors that have synergistic effects on many of their health issues.
Discussion
This thematic analysis synthetized the theoretical and empirical literature on the characteristics of self-management of patients with complex healthcare needs. This clientele presents additional self-management challenges in regard to: the prioritization of self-care, a greater risk for depression or psychological distress, a greater risk of poor self-efficacy and the risk of receiving conflicting information from healthcare professionals. However, they can rely on their knowledge and previous experience gained in other situations (Coventry et al., 2014).
Liddy et al. (2014), conducted a literature review aiming to explore barriers to self-management through the perspective of patients living with multiple chronic conditions. Of the 21 articles used in our thematic analysis, seven of them were also included in their review. Common themes emerged from both studies, such as contradictory information and high risk for depression. Our analysis also highlights other particularities such as poor self-efficacy, often observed in this clientele, and the fact that patients frequently rely on past experience to adequately take charge of their health.
One of the main challenges of self-management is the prioritization of self-care. Patients with numerous chronic diseases are constantly confronted with having to make choices amongst the care activities to prioritize. Most will identify a dominant disorder on which to focus their efforts (Bratzke et al., 2015). In certain situations, the characteristics of a condition are in conflict with the management of others and the successful management of a condition can hinder the taking in hand of another (Sharry, Bishop, Moss-Morris, & Kendrick, 2013). Patients will more easily accept to engage in self-care activities that they consider beneficial to more than one of their conditions (Bayliss, Ellis, et al., 2007; Bower et al., 2013; Leach & Schoenberg, 2008). Social issues and economic situations will influence how patients prioritize self-care (Bosworth, Powers, & Oddone, 2010). The healthcare provider can explore the reasons that guide this prioritization for a given patient. Interventions may have a greater impact if the healthcare provider takes time to explain the benefits of self-management behaviours for the different conditions facing the patient. Depression and emotional distress may impair self-management by decreasing motivation, prioritization skills and problem-solving. Negative emotions may also decrease self-confidence and self-efficacy (Lin, Burgess Jr, & Carey, 2012) and distress is often present in this vulnerable clientele (Dinkel, Schneider, Schmutzer, Brähler, & Häuser, 2016; Fortin et al., 2006). Healthcare providers must remain vigilant during their self-management support activities with this clientele, for the quick detection of psychological distress and the treatment of mental health issues.
Patients with complex care needs reported receiving conflicting information from the health professionals they consulted. Between 25% and 80% of patients received contradictory information on their diseases and their management (Elstad, Carpenter, Devellis, & Blalock, 2012). Receiving conflicting information from two sources that the person trusts can complicate self-management (Elstad et al., 2012). In order to help these patients as much as possible, it is important that healthcare providers offer a personalized evaluation of their needs, as well as proper follow-up, and ensure good coordination between their various health professionals (Noel et al., 2007). Healthcare providers can ensure coordination of the information provided by various health professionals involved in the patient’s follow-up.
Although the majority of studies report that complexity is an additional challenge to self-management, the coexistence of many chronic conditions can also become an opportunity to call on past learning experiences (Vellone et al., 2013). The healthcare provider can help the patient become aware of the knowledge and skills gained in the past as well as positive experiences.
Limitations Our study presents some limitations. There is a lack of consensus in the literature regarding the definition of patients with complex needs. We ensured that the selection criteria developed for this study were broad enough to include a range of definitions for complexity. A limitation of any review is the potential omission of relevant articles as well as any unpublished material. However, all necessary measures were taken to ensure an exhaustive document review: our search strategy was adapted to various databases and was developed in collaboration with an information specialist. Furthermore, we identified additional papers by hand search.
Conclusions
Patients with complex healthcare needs are confronted with extra challenges with self-management, these being exacerbated in the presence of socioeconomic insecurity. These patients must often prioritize self-care according to one dominant condition. They are more at risk for depression, psychological distress and low self-efficacy, as well as for receiving contradictory information from healthcare providers. On the other hand, their previous experiences may help them improve their self-management skills. Future studies could empirically validate the results of this research and contribute to the understanding of the experience of these patients. Healthcare providers can learn from these results to better adapt their self-management support interventions to meet the specific needs of this vulnerable clientele.
Type d’étude
La recherche qualitative de type descriptive simple (Fortin & Gagnon, 2016) est le devis utilisé pour cette étude. Celle-ci vise à décrire un phénomène en particulier; elle fournit de l’information sur les caractéristiques, les comportements et les conditions des personnes et elle permet la description d’un concept relatif à une population (Fortin & Gagnon, 2016). Cette recherche qualitative descriptive a été réalisée sous forme exploratoire puisqu’il s’agit d’un projet de mémoire et qu’une analyse thématique a également été réalisée préalablement sur le sujet (Gray, Grove, & Suttherland, 2017).
Population cible et échantillon La population cible de cette étude est constituée de toutes les personnes ayant des besoins de santé complexes qui fréquentent les services de soins de santé du Québec. La population accessible est constituée de personnes ayant des besoins de santé complexes qui fréquentent les services de soins de santé du Saguenay-Lac-Saint-Jean, notamment celle présentant une grande utilisation des services d’urgence ou d’hospitalisations.
L’échantillon de 10 participants a été recruté à partir de la liste de patients ciblés par le Centre intégré universitaire de santé et de services sociaux (CIUSSS) du Saguenay-Lac-Saint-Jean comme étant de grands utilisateurs des services de soins de santé, selon les critères du CIUSSS, soit avec six visites à l’urgence et/ou trois hospitalisations ou plus dans une année, et à qui, suite à l’évaluation de leur dossier par les gestionnaires de cas du programme de grands utilisateurs du CIUSSS, ont été jugés admissibles au programme de gestion de cas en raison de la complexité de leurs besoins. Cela ne constitue pas une population uniforme car, tel qu’expliqué dans les chapitres précédents, la situation de complexité des besoins de santé d’une personne est tributaire de plusieurs facteurs reliés, à la fois, à sa condition de santé et à d’autres facteurs psychosociaux et économiques. Néanmoins, il est reconnu dans la littérature que les personnes présentant une utilisation accrue de services de santé sont représentatives d’une population présentant des besoins de santé complexes (Poremski et al., 2016). Puisque la recherche se déroule dans le cadre d’un projet de maitrise et qu’une analyse thématique de la littérature a également été réalisée et soumise pour publication, nécessitant ainsi un investissement de temps important, il a été décidé de limiter l’échantillon à 10 participants pour pouvoir respecter les échéanciers. Cependant, l’équipe de recherche prévoit éventuellement poursuivre sa collecte de données à l’extérieur du cadre du présent mémoire.
Procédure d’échantillonnage Trouver des participants ayant des besoins de santé complexes pour participer à cette étude s’est avéré être un défi. En ce sens, l’échantillonnage s’est fait par choix raisonné (Fortin & Gagnon, 2016) à partir d’une liste établie par le CIUSSS du Saguenay-Lac-Saint-Jean, des personnes considérées comme des grands utilisateurs des services de soins de santé. Les participants répondant aux critères d’inclusion et d’exclusion ont été ciblés sur la liste par les gestionnaires de cas (infirmière ou travailleuse sociale) oeuvrant dans le programme de gestion de cas des grands utilisateurs dans l’un des six territoires du CIUSSS, puis ceux-ci demandaient l’autorisation aux personnes ciblées d’être contactées par l’équipe de recherche. Les critères d’inclusion étaient les suivants : 1) être âgé 18 ans ou plus; 2) être sur la liste des grands utilisateurs du CIUSSS du Saguenay-Lac-Saint-Jean; 3) comprendre et s’exprimer en français. Les personnes avec des troubles cognitifs ou des maladies mentales décompensées étaient exclus. L’échantillon a été formé d’hommes et de femmes, et il y a eu une diversité de profils et de milieux, parmi les participants choisis. Il s’agit d’une population accessible et qui correspond au profil recherché (Fortin & Gagnon, 2016). Tous les patients qui ont été référés à l’étudiante-chercheure par les gestionnaires de cas ont accepté de participer au projet.
Description de la méthode de collecte de données
La collecte de données s’est faite sous forme d’entrevue individuelle semi-dirigée. Les participants ont été référés par les gestionnaires de cas du CIUSSS du Saguenay-
Lac-Saint-Jean suite à l’accord obtenu de la coordonnatrice régionale du continuum des soins, puis rejoints par l’étudiante-chercheure. Les entrevues se sont déroulées de mai à septembre 2017, elles étaient d’une durée approximative de 45 minutes et ont été faites par l’étudiante-chercheure. Afin d’élaborer le guide d’entrevue, les questions ont été développées dans le but d’explorer les trois domaines de tâches et les six compétences essentielles d’autogestion du modèle théorique de Lorig et Holman (2003) (voir Appendice A). Les questions du guide d’entrevues ont été pré-testées et validées auprès des deux patients partenaires afin de s’assurer que celles-ci étaient claires et pertinentes. Les entrevues ont eu lieu à domicile et dans les locaux du CIUSSS du Saguenay-Lac-Saint-Jean, à la convenance du participant. Les principaux obstacles lors de la collecte de données ont été la difficulté à prévoir un moment pour rencontrer les patients vu leurs nombreuses occupations et rendez-vous médicales. Également, la présence d’un conjoint durant l’une des entrevues a rendu celle-ci plus complexe. Aussi, une fiche signalétique comportant des questions afin de décrire les caractéristiques sociodémographiques des participants était complétée (voir Appendice B).
Plan d’analyse des données
L’analyse des données a été effectuée à l’aide du logiciel NVivo (version 11). L’analyse a été réalisée en trois étapes pour toutes les entrevues : 1) condensation des données; 2) présentation des données; et 3) formulation et vérification des conclusions (Miles et al., 2014). De plus, l’analyse a été fait en utilisant un codage mixte tel que décrit par Miles et al. (2014), en se basant sur les trois domaines de tâches et les six compétences d’autogestions définis dans le modèle de Lorig et Holman (2003). Toutes les entrevues ont été codifiées dans le logiciel NVivo. Puis, pour faciliter l’analyse, celle-ci a été faite sous forme de matrices grâce à ce même logiciel. Un croisement a donc été créé entre les trois domaines de tâches et les six compétences d’autogestion du modèle de Lorig et Holman (2003), permettant ainsi de classer les extraits des transcriptions d’entrevues correspondant à chacune des compétences d’autogestion qui comportaient une spécificité chez la clientèle à l’étude.
Critères de rigueur
Pour assurer la fiabilité, les données trouvées pour chaque compétence ont été revues par la directrice et la co-directrice du mémoire afin de s’assurer que les extraits de transcriptions des entrevues soient classés dans le bon thème analytique. Les désaccords et les questions ont été discutés et l’analyse a également été validée dans son ensemble par la directrice et la co-directrice du mémoire. Le fait que les entrevues aient toutes été réalisées par la même personne (l’étudiante-chercheure) a favorisé la crédibilité. En notant et en enregistrant toutes les transcriptions telles que mentionnées par les participants lors des entrevues dans le logiciel NVivo 11, la confirmabilité a été assurée. De plus, la transférabilité est également respectée puisque les caractéristiques des participants sont bien décrites dans la section résultats.
Considérations éthiques
Cette étude a été approuvée par le Comité d’éthique de la recherche du CIUSSS du Saguenay-Lac-Saint-Jean (voir Appendice C), en vertu de l’entente UQAC et CIUSSS du Saguenay-Lac-St-Jean (http://recherche.uqac.ca/entente-uqac-et-csss-de-chicoutimi/). Un consentement libre, éclairé et continu a été obtenu par l’étudiante-chercheure. Le projet de recherche a été expliqué en profondeur aux participants afin que ceux-ci puissent évaluer convenablement les risques et bénéfices de leur participation. Des explications claires et précises ont été données, dans un langage adapté, et les participants ont eu tout le temps nécessaire pour lire le formulaire d’information et de consentement (voir Appendice D).
Résultats
Les caractéristiques des participants ainsi que les résultats obtenus suite à l’analyse des entrevues individuelles sont présentés dans ce chapitre. Les thèmes généraux qui ont émergé des entrevues individuelles ont été regroupés selon les six compétences d’autogestion du modèle de Lorig et Holman (2003). Pour la présentation des résultats, les trois domaines de tâches du modèle théorique ont été intégrés directement dans la description des compétences.
Caractéristiques des participants
Au total, dix participants ont été interviewés. Le Tableau 1 présente les principales caractéristiques des participants. Les participants étaient des personnes ayant des besoins de santé complexes demeurant sur le territoire du Saguenay-Lac-Saint-Jean. Comme la très grande majorité de la population de cette région, tous les participants étaient de nationalité québécoise. Sept sur dix étaient des femmes. La moyenne d’âge était de 65,4 ans. Six sur dix avaient complété leurs études secondaires. Six sur 10 étaient déclarés invalides en raison de leurs problèmes de santé. Cinq étaient mariés. Quatre d’entre eux avaient un revenu familial supérieur à 60 000$, alors que quatre autres avaient un revenu familial inférieur à 20 000$.
Caractéristiques de l’autogestion des participants
Mise en action
Faire des actions pour prendre sa santé en main semble être très ardu pour les participants. Leur quotidien est rempli de tâches à réaliser, mais plusieurs ne semblent malheureusement pas parvenir à toutes les accomplir. En effet, certains rapportent se sentir constamment épuisés, fatigués ou stressés, ce qui leur procure un sentiment d’incapacité par rapport aux soins qu’exigent leurs problèmes de santé. Bien qu’ils connaissent l’importance de bien prendre leur médication, de bien manger, de faire de l’exercice, bref de suivre leur plan de traitement, chaque soin leur demande beaucoup d’énergie; ils ont souvent beaucoup de difficultés à les accomplir.
Non, c’est sûr que je pourrais mieux m’occuper de moi, mais depuis les Fêtes, j’ai une faiblesse terrible, je ne suis plus capable.
Oui, je veux marcher, je veux aller m’entrainer, mais je me demande comment je vais faire honnêtement. Je ne suis pas capable, je suis trop fatiguée.
Étant vulnérables, ces personnes vivent également beaucoup de stress et d’inquiétude par rapport aux activités de soins que requièrent leur situation de santé. Elles peuvent même, pour certaines, sombrer dans la dépression lorsqu’elles sentent que la planification et la mise en place des actions qu’exige l’autogestion de leur maladie prennent trop de place et dépassent leurs compétences.
|
Table des matières
Liste des tableaux et des figures
Liste des tableaux et des figures
Liste des abréviations et des sigles
Introduction
Chapitre 1 : Problématique
Problème
Cadre théorique
But de l’étude et question de recherche
Chapitre 2 : Recension des écrits
Characteristics of self-management among patients with complex health needs: a thematic analysis review
Abstract
Strengths and limitations of this study
Introduction
Methods
Design
Search methods
Data collection
Analysis and synthesis
Results
Included studies
Characteristics of self-management by patients with complex health needs
Discussion
Limitations
Conclusions
Declarations
Acknowledgements
Authors’ contributions
Competing interests
Patient consent
Provenance and peer-review
Funding
References
Chapitre 3 : Méthodologie
Type d’étude
Population cible et échantillon
Procédure d’échantillonnage
Description de la méthode de collecte de données
Plan d’analyse des données
Critères de rigueur
Considérations éthiques
Chapitre 4 : Résultats
Caractéristiques des participants
Caractéristiques de l’autogestion des participants
Mise en action
Prise de décision
Développement d’un partenariat patient-intervenant
Auto-adaptation
Utilisation des ressources
Résolution de problèmes
Synthèse des principaux résultats
Chapitre 5 : Discussion
Discussion des résultats
Modèle théorique
Forces et limites
Échantillonnage
Collecte de données
Analyse des données
Retombées attendues
Pour la recherche
Pour la pratique
Pour la formation
Conclusion
Références
Appendice A : Guide d’entrevue
Appendice B : Fiche signalétique
Appendice C : Approbation éthique final
Appendice D : Formulaire d’information et de consentement
![]() Télécharger le rapport complet
Télécharger le rapport complet